Our Mission
At LinkMD, we’re on a quest to reinvent the entire Revenue Cycle Management (RCM) journey—from the moment a patient checks in to the final resolution of a claim—by leveraging an ecosystem of AI-driven agents. We consistently hear from our clients and partners about the challenges of securing prior authorizations (PAs) for treatments, coping with limited staff for appeals, and trying to manage the entire PA submission process across large organizations. These hurdles often lead to delayed or denied reimbursements—and worse yet, they can disrupt patient care.
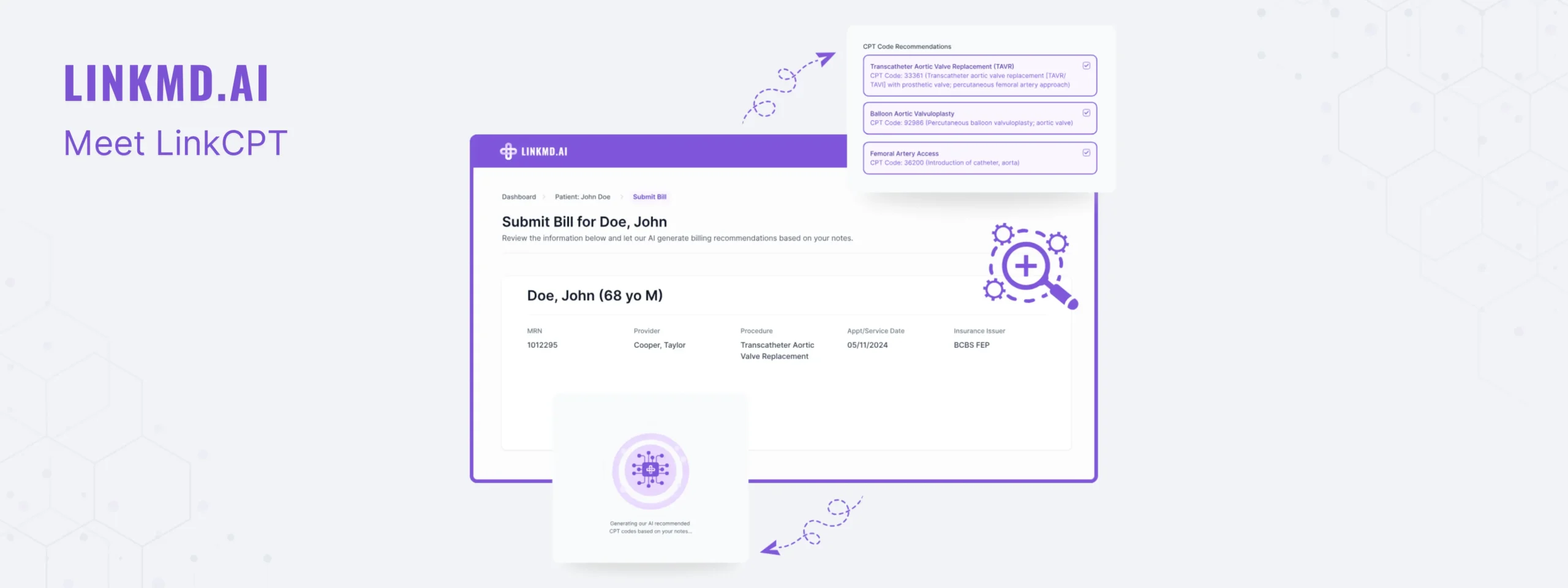
With coding guidelines and payer policies evolving at a dizzying pace, providers struggle to keep up with ever-changing CPT code updates and compliance requirements. That’s when our team asked a critical question: “How can we build AI agents that code accurately, optimize clinical documentation to match payer guidelines, and ensure providers receive full reimbursement for the services they deliver?” By integrating automation, intelligent data analysis, and efficient workflows, we aim to cut through administrative clutter, unearth actionable insights from claims data, and give healthcare professionals the freedom to focus on delivering the best possible patient care.
RCM Landscape
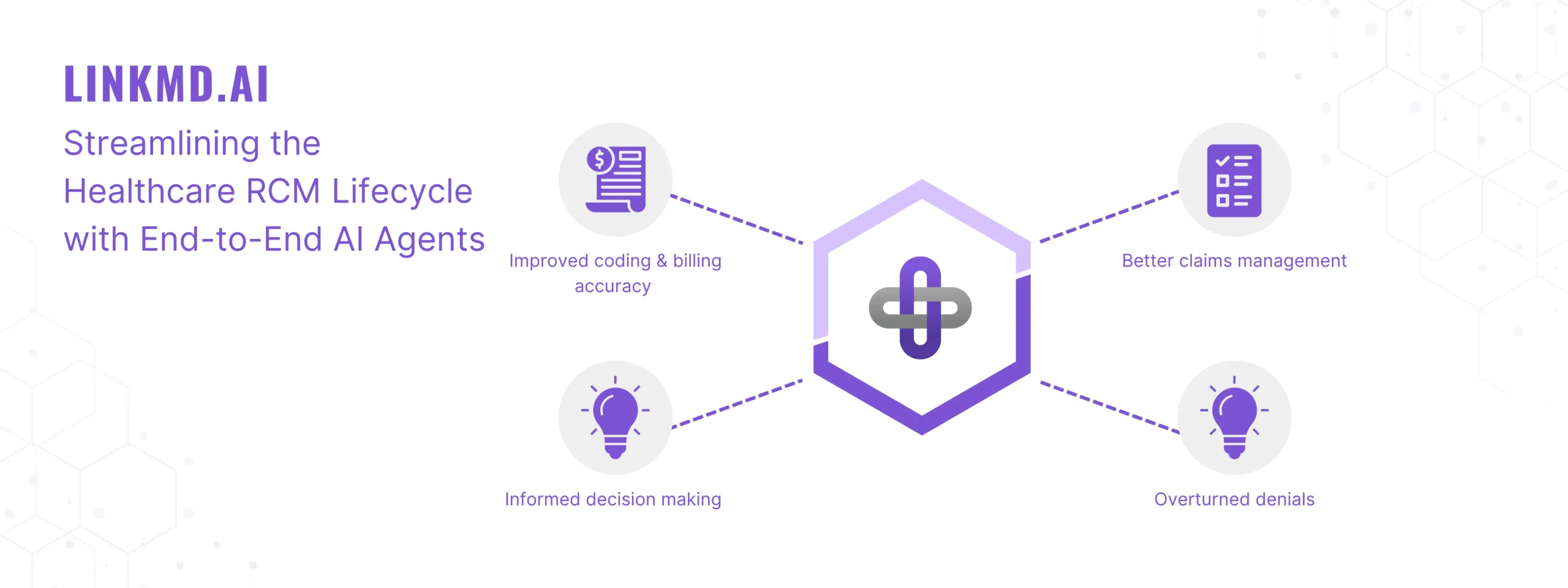
The current RCM process is tangled with manual tasks, fragmented data, and constant payer rule changes—all of which strain providers who already have their hands full caring for patients. Each step, from patient registration through coding, billing, and collections, can introduce errors and bottlenecks, fueling frustration on both sides. Providers and health systems often wonder, “How do I make sense of my claim data? Where am I losing money, and how can I learn from it?” That’s why LinkMD is building a comprehensive ecosystem of AI-driven solutions for every phase of the RCM lifecycle—streamlining PAs, staying on top of ever-evolving coding guidelines, and offering robust analytics, reporting, and strategic decision-making tools. By tackling administrative obstacles head-on, we’re helping providers reduce denials, minimize revenue leaks, and spend more time doing what they do best: caring for patients.
How LinkMD Transforms the RCM Lifecycle with Patent Pending Technology
Pre-Service Optimization
- Automated Prior Authorizations & Tracking: Our patent-pending AI technology revolutionizes the prior authorization process by fully automating submissions and managing denials effortlessly. With our all-in-one platform, you can submit, track, and organize prior authorizations in seconds, saving time and eliminating manual hassle.
- Automated Eligibility & Benefit Verification: Real-time checks ensure patients’ coverage details are confirmed up front. This proactive approach minimizes administrative surprises later in the cycle, saving time and resources for both providers and patients.
Service Simplification
- AI-Driven Coding & Documentation: Automated workflows ensure accuracy in coding and documentation, reducing the burden on clinical staff. By guiding users through best practices, errors are minimized, and compliance is improved—all while saving valuable time.
Billing & Payment Streamlining
- Automated Claim Submissions: Our AI agent automatically gathers all relevant patient information and provider documentation to build a complete claim, maximizing the chances for approval and reimbursement. An AI-powered checklist guides billers and staff before claims are submitted, ensuring accuracy and efficiency
- Denial Management & Pattern Recognition: Address denials immediately with automated letters of appeal. Our AI clarifies why each claim was denied and recommends the most effective steps to resolve the issue, helping you reclaim valuable revenue faster
- Pattern Recognition: Advanced analytics pinpoint potential denial trends and risk factors before claims are even filed. By proactively addressing these root causes, providers can significantly reduce denials and associated costs. A built-in confidence scoring system suggests the best course of action for achieving successful claim outcomes.
- Financial Audits & Insights: Integrated auditing tools detect anomalies early, safeguarding your financial health and streamlining resolutions when concerns arise. With detailed, data-driven insights, providers can optimize their processes and maintain smooth revenue cycles.
Looking Ahead
Over the coming weeks, we’ll dive deeper into each stage of the RCM lifecycle to show how LinkMD’s AI Agentic Ecosystem can help providers thrive in a complex healthcare landscape. From pre-service optimizations that reduce administrative hurdles to post-payment analytics that highlight new opportunities for growth, we’ll explore how AI-driven solutions can redefine efficiency, reliability, and—ultimately—patient satisfaction.
Stay tuned for more insights, and discover how you can partner with LinkMD to transform your RCM process from end to end.