Picture this: A worried father paces in a sterile hospital waiting room while his daughter—a young woman with a chronic condition—endures another episode of debilitating symptoms. Her physician has found a promising new procedure that could ease her suffering, but there’s one hurdle: It requires prior authorization. Days turn into weeks as the care team battles a maze of forms, phone calls, and re-submissions. Meanwhile, her condition worsens and her family’s anxiety grows.
This scenario, unfortunately, is all too familiar to clinicians, patients, and caretakers alike. Prior authorization (PA)—the process through which a healthcare provider obtains approval from a health insurer before proceeding with a specific treatment, medication, or procedure—was originally introduced as a cost-containment measure. Over the past decade, however, the process has evolved into a significant administrative burden that can delay crucial patient care.
The Landscape of Prior Authorizations
Rising Complexity: Prior authorization processes were once limited to only the most expensive or novel treatments. Today, they encompass a broad spectrum of healthcare services, from advanced imaging and specialty medications to routine diagnostic tests. A 2022 survey by the American Medical Association (AMA) reported that over 90% of physicians describe prior authorization requirements as “high or extremely high” in terms of administrative burden.
Increased Volume: According to a 2021 Council for Affordable Quality Healthcare (CAQH) Index, healthcare providers and payers spend upwards of $33 billion annually on prior authorization tasks alone. These tasks include phone calls, faxing documents, and repetitive form completions—a stark indication of how deeply PA has penetrated the day-to-day workflow in clinical settings.
Regulatory Attempts: Recognizing the growing burden, regulatory agencies and industry groups have proposed reforms. In late 2022, the Centers for Medicare & Medicaid Services (CMS) proposed rules to streamline prior authorization by mandating shorter turnaround times and establishing standardized data exchange. While these moves signal optimism, real-world implementation has been patchy. Providers often still face scattered, inconsistent requirements from different insurance plans.
Challenges from the Clinical Standpoint
Administrative Overload and Burnout: Many physicians cite the process of obtaining prior authorizations as a primary contributor to professional burnout. It’s not uncommon for a physician’s staff to spend hours each day on hold, waiting to speak to insurance representatives, or resubmitting documentation for a single patient’s approval. These tasks translate into lost clinical hours—time that could be spent diagnosing patients or discussing treatment options.
- Paperwork Over Patient Work: The AMA’s 2021 Prior Authorization Physician Survey found that doctors complete an average of 41 prior authorizations per week, taking nearly 13 hours of physician and staff time.
Fragmented and Conflicting Requirements: Different insurance carriers often have different criteria for approvals, and these criteria can change without much warning. Clinicians may discover mid-treatment that a plan no longer covers a certain medication unless a new form is submitted—further delaying care.
- Ever-Changing Goalposts: A previously approved medication might suddenly require new clinical justification. This unpredictability complicates treatment planning and can erode patient trust when their care is suddenly disrupted.
Clinical Judgment Undermined: Physicians train for years to make evidence-based decisions tailored to individual patient needs. Prior authorization can reduce that autonomy, as insurers may request alternative treatments that may not align with the clinician’s best judgment.
- One-Size-Fits-All: A treatment that works for one patient might be wholly inadequate for another. Yet, providers must often “fail” a cheaper or generic medication before trying the drug initially recommended. This “step therapy” protocol can extend suffering and delay relief.
The Human Cost: Delayed Patient Care
Every hour or day of delay can make a life-altering difference for a patient. A 2022 American Hospital Association (AHA) report found that nearly 60% of delayed hospital discharges were partially attributable to prior authorization hold-ups. Meanwhile, the AMA reports that 94% of physicians say prior authorizations lead to delayed patient care, and 24% say it has led to a serious adverse event for a patient in their care.
Harm to Patients with Chronic Illnesses: For individuals living with diabetes, rheumatoid arthritis, or severe mental health disorders, timely treatment is critical. A prior authorization that languishes for weeks can mean hospital readmissions, exacerbation of symptoms, and a downturn in quality of life.
Emotional Toll: Beyond clinical outcomes, families experience deep frustration, stress, and financial worry when treatments are paused. Patients who’ve prepared emotionally for a procedure or pinned their hopes on a new medication often feel betrayed by a system that seems to value bureaucracy over care.
Erosion of Trust: When approvals are delayed or denied, patients sometimes perceive their healthcare providers as complicit in the red tape. Physicians frequently share in patients’ frustration, but the complexity of insurance requirements hinders transparent communication and swift action.
Toward a Better Future
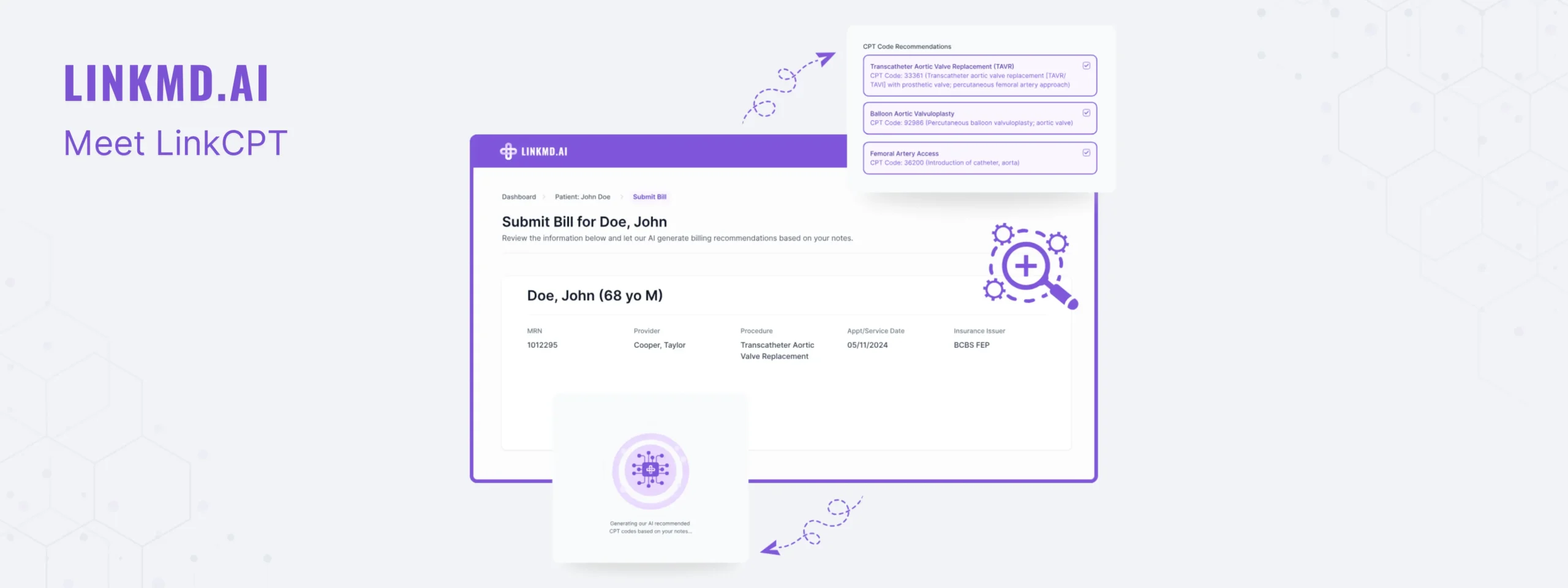
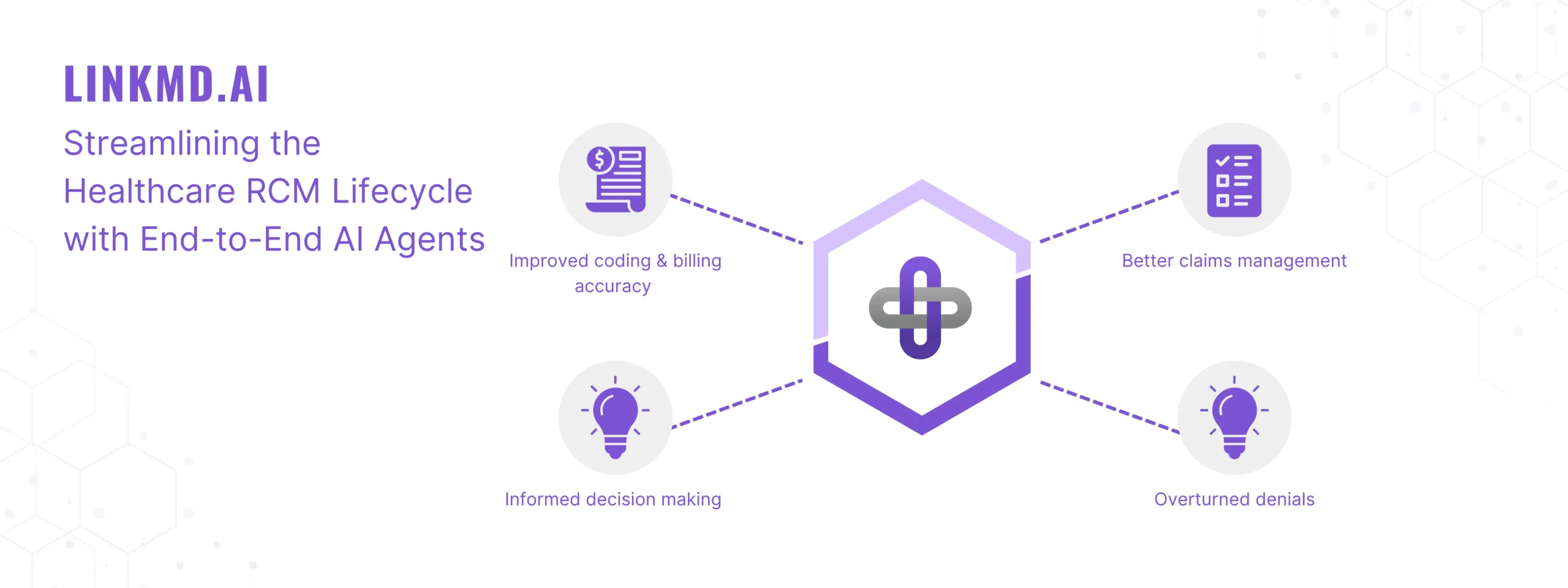
Technological Solutions: Electronic prior authorization (ePA) platforms promise to streamline workflows. By integrating PA directly into electronic health record (EHR) systems, providers can populate forms with existing patient data, reducing redundancy. According to CAQH, even a modest increase in the adoption of automated processes could save the healthcare industry billions each year and cut approval times by half or more.
Policy Revisions: Momentum is growing for more standardized, transparent rules regarding prior authorization. Medical societies, patient advocacy groups, and hospital associations are pushing for legislation that would set maximum response times and require insurers to publicly share their coverage criteria.
Collaboration & Education: Insurers and providers must work together to align clinical guidelines with reimbursement policies. Regular communication and shared data regarding best practices can help reduce the need for repeated paperwork. Similarly, educating patients about their insurance plans, what services are likely to require authorization, and how to expedite the process can help manage expectations and limit surprises.
Conclusion: The Imperative for Change
While prior authorization was created to curb unnecessary costs and protect patients from expensive or unproven treatments, its ballooning complexity has yielded a new set of challenges. The stories of delayed surgeries, denied medications, and burnt-out clinicians spotlight the need for urgent reforms.
Ultimately, streamlining and modernizing prior authorization processes has benefits for everyone. Patients receive more timely treatments. Clinicians can focus on patient care instead of battling bureaucratic red tape. And payers can still manage costs effectively while improving provider relations and patient satisfaction.
In healthcare, time is more than money—it’s often the difference between a patient’s rapid recovery and chronic disability, between hope and despair. By acknowledging the burden of prior authorizations and working collaboratively to implement lasting solutions, we can restore the balance between cost management and compassionate, patient-centered care.
References (Suggested Reading):
- American Medical Association (AMA). 2021 AMA Prior Authorization Physician Survey.
- Council for Affordable Quality Healthcare (CAQH). 2021 CAQH Index.
- American Hospital Association (AHA). Reports on Delays in Patient Care due to Prior Authorizations.
- Centers for Medicare & Medicaid Services (CMS). Proposed Rules on Streamlining Prior Authorization (2022).