Managing the revenue cycle has always been a tightrope walk for healthcare organizations. On one side, you have soaring patient volumes, complex regulations, and the constant need to maintain compliance. On the other side, you must keep operations efficient while delivering the highest quality patient care. The result? A delicate balancing act that often leaves billing teams overwhelmed, patients frustrated, and finances stretched thin.
Enter end-to-end AI automation—a transformative approach that promises to bring much-needed relief to stressed RCM departments. In this post, we’ll explore the common pain points in the healthcare RCM space and then take a closer look at how LinkMD.ai leverages specialized “agents” to streamline the entire revenue cycle management process in a more efficient and patient-friendly way.
Understanding the Core Challenges in RCM
- Prior Authorization Hurdles: For many clinics, obtaining prior authorizations (PAs) is a bottleneck. The back-and-forth with payers can lead to delays, rescheduled appointments, and potential revenue losses if authorization isn’t secured quickly.
- High Denial Rates: From coding issues to missing documentation, there are many reasons a claim can be denied. Each denial typically requires time-consuming investigation, appeal, and resubmission—leading to added stress for staff, extended days in accounts receivable, and lost revenue.
- Complex Appeals Processes: Crafting compelling appeal letters—often referred to as Letters of Medical Necessity—can be difficult if you lack a centralized resource to guide you through payer requirements and up-to-date clinical evidence. If not done carefully, even legitimate claims can be rejected multiple times.
- Unclear Insurance Eligibility: Unverified coverage or inaccurate benefit checks often surface well into treatment, leaving clinics vulnerable to increased denials and patients with unexpected bills. When neither staff nor patients have a clear view of coverage details, confusion—and costs—rapidly escalate.
- Incomplete or Inaccurate Coding: Healthcare coding isn’t just about administrative housekeeping—it’s directly tied to your organization’s bottom line. Even minor coding errors or missed CPT codes can mean denied claims, underpayments, or compliance infractions.
How LinkMD.ai Transforms RCM with Specialized AI “Agents”
To address these challenges holistically, LinkMD.ai has developed a suite of AI-driven “agents,” each targeting a specific piece of the RCM puzzle. Rather than patch together multiple disparate solutions, LinkMD.ai unites them under one intelligent platform—driving down errors, accelerating workflows, and freeing up staff to focus on patient care.
Below is a closer look at LinkMD.ai’s agents and how they tackle key RCM pain points:
Authorization AI
- What It Does: Handles prior authorizations quickly and seamlessly.
- Key Benefit: Submitting requests can take mere seconds, and real-time tracking keeps you constantly informed of a patient’s PA status.
- Why It Matters: By automating and expediting this notoriously tedious step, clinics see fewer scheduling delays, faster approvals, and greater transparency—all of which translate into improved patient experiences and more reliable revenue streams.
Billing Denial Root Cause Agent
- What It Does: Analyzes denied claims to pinpoint exactly what went wrong.
- Key Benefit: Identifies patterns behind denials—such as coding mistakes or missing documentation—so billing teams can address them right away.
- Why It Matters: By tackling root causes, this agent not only rescues current claims but also prevents the same issues from cropping up again, effectively boosting future approval rates and shortening the denial management cycle.
Letter of Necessity Agent
- What It Does: Learns dynamically from previous denials and outcomes to craft stronger, data-driven appeal letters.
- Key Benefit: Pulls reliable information from trusted sources like NIH and PubMed, ensuring each appeal is backed by up-to-date clinical research.
- Why It Matters: Thoughtful, evidence-based letters of necessity significantly increase the chance of claim approval and reduce the back-and-forth with payers. This helps clinics not only improve revenue but also maintain good payer relationships.
Eligibility AI
- What It Does: Offers a clear and upfront view of a patient’s insurance coverage and benefits before services are rendered.
- Key Benefit: Minimizes surprises by confirming coverage details early, reducing denials, and preventing patient dissatisfaction over unforeseen costs.
- Why It Matters: With real-time eligibility insights, clinics can plan treatments more confidently, improving both financial health and patient satisfaction in the process.
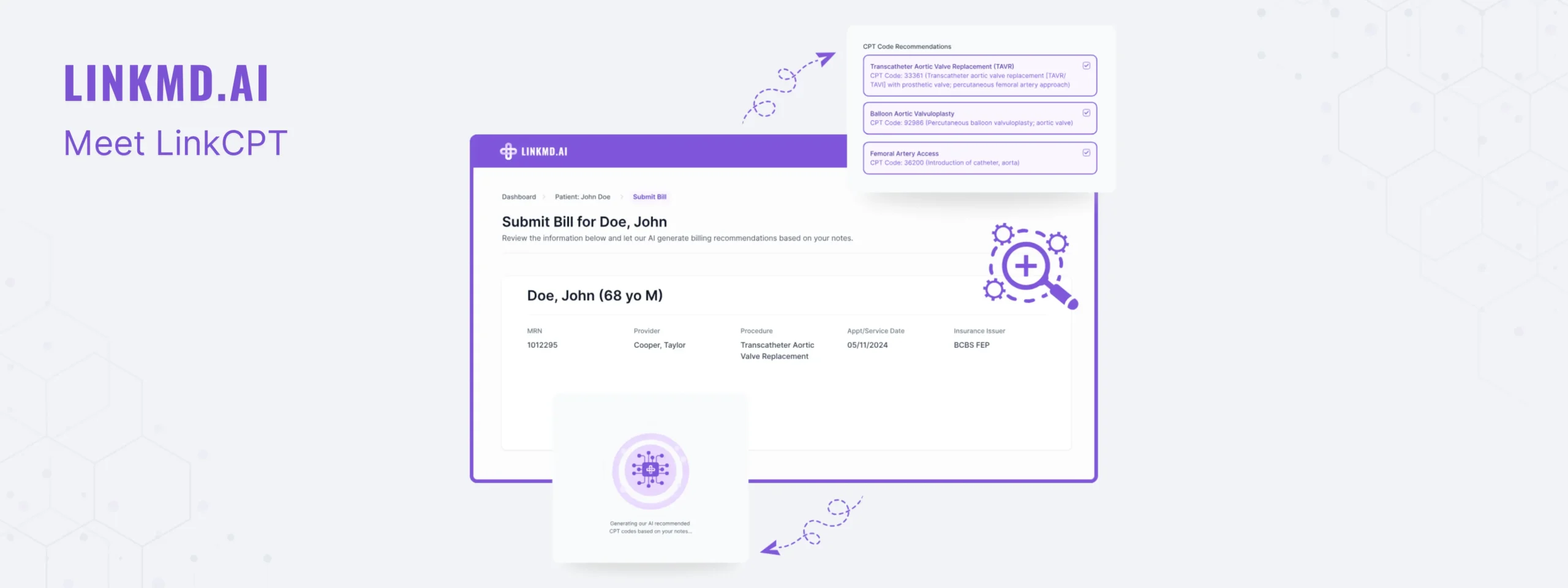
CPT AI
- What It Does: Ensures accurate and complete coding by leveraging AI to analyze clinical documentation.
- Key Benefit: Suggests potential CPT codes and flags missed billing opportunities, streamlining the coding process and safeguarding against errors.
- Why It Matters: Precise coding is the bedrock of timely, reliable reimbursements. By automating this step, you not only decrease denial rates but also optimize revenue capture—allowing staff to refocus on patient care rather than billing disputes.
Bringing It All Together: A Unified Approach to RCM
One of the biggest advantages of implementing the LinkMD.ai platform is that all these agents work in tandem. Rather than juggling multiple software tools that each address a narrow part of the revenue cycle, LinkMD.ai offers an end-to-end solution, powered by integrated AI. Here’s what this means in practice:
- Improved Operational Efficiency: Fewer manual touchpoints mean fewer opportunities for errors and more time for staff to engage in patient-centered tasks.
- Faster Reimbursements: Proactive denial management and real-time eligibility checks reduce lengthy appeals and claims rework.
- Cost Savings: By cutting down on administrative overhead, clinics see immediate savings in both time and resources.
- Enhanced Patient Satisfaction: When patients experience fewer billing mistakes and easier-to-understand statements, they’re more likely to trust and remain loyal to your clinic.
- Continuous Learning: Each agent’s AI framework continually refines its approach based on new data, ensuring you’re always improving and adapting to payer trends and regulatory changes.
Why the Time Is Now
Healthcare is an industry in constant flux—regulations change, payer policies evolve, and patient expectations keep rising. Relying on legacy systems or manual processes simply isn’t sustainable if you want to remain financially healthy and patient-focused in the long run.
With an end-to-end AI automation solution like LinkMD.ai, clinics can finally bridge the gap between quality care and efficient, reliable revenue cycle management. It’s not just about collecting payments faster; it’s about creating an environment where administrative hurdles no longer stand in the way of delivering the best possible patient experience.