In today’s rapidly evolving healthcare landscape, one administrative process continues to consume an outsized share of time, money, and mental bandwidth for providers and payers alike: prior authorization. Often cited as the biggest bottleneck to efficient care delivery, prior authorization can create frustrating barriers for both clinicians and patients. However, thanks to emerging digital technologies and forward-thinking solutions — like those championed by LinkMD — this longstanding challenge is on the cusp of a transformative overhaul. Here’s how technology is reshaping the future of prior authorization and unlocking new frontiers in healthcare efficiency.
The Current State of Prior Authorization
Inefficiencies and Frustrations
Traditionally, prior authorization has been synonymous with administrative bottlenecks: extensive paperwork, time-consuming phone calls, lengthy approval wait times, and a lack of transparency into where a request stands. On average, it can take hours or even days for healthcare providers to receive approval, delaying critical patient treatments or tests.
The Impact on Provider Burnout
Physicians and their staff invest significant time following up with payers and completing repetitive documentation. This administrative burden contributes heavily to provider burnout, an ongoing concern that drives many professionals away from clinical practice. In a system where every second counts, these manual workflows are both costly and unsustainable.
The Technology-Driven Revolution
Automation and Artificial Intelligence
Technological tools, particularly automation and artificial intelligence (AI), are revolutionizing prior authorization by streamlining the information-exchange process and eliminating many of the manual tasks that plague traditional workflows. Here’s how:
- Automated Document Collection: Systems that can automatically gather a patient’s relevant medical documentation, lab results, and imaging studies directly from the electronic health record (EHR) free up valuable time for clinical and support staff.
- AI-Powered Decision Support: AI-driven algorithms can review patient data against payer-specific guidelines, determining the likelihood of approval before an official request is even submitted. This pre-check process reduces errors, prevents unnecessary denials, and speeds up approvals.
- Smart Forms and Templates: Digital platforms generate dynamic forms that prompt care teams to provide precisely the information needed for each unique request. This prevents missing or extraneous data and accelerates approvals.
Interoperability and Data Sharing
To transform prior authorization into a nimble, intelligent process, interoperability is key. Modern healthcare demands seamless data exchange among EHRs, payer portals, and third-party systems. Initiatives like FHIR (Fast Healthcare Interoperability Resources) standards allow for more efficient and secure data transfers, ensuring patient information is consistent and accurate across platforms.
When providers and payers can communicate and exchange information in real-time, the entire prior authorization cycle shortens from days to mere hours—or less. Reduced wait times not only enhance patient satisfaction but also free clinicians to focus on delivering higher-quality care.
Regulatory Changes and Industry Momentum
Legislative Push
Regulators, aware of the burdens associated with prior authorization, are pursuing measures that encourage greater transparency and faster approvals. New rules from the Centers for Medicare & Medicaid Services (CMS) and state legislatures underscore the urgency of automated solutions and standardized requirements. For example, CMS has introduced proposals that mandate electronic prior authorization and timelines for payer responses, ensuring an environment more conducive to technology-driven transformations.
Healthcare Innovation Boom
Additionally, a wave of innovation is sweeping through the healthcare industry. Venture capital and corporate investments in HealthTech solutions hit record highs in recent years, accelerating the development of sophisticated systems aimed at making prior authorization more efficient and less error-prone.
Harnessing Technology for Better Healthcare Efficiency
The Role of LinkMD
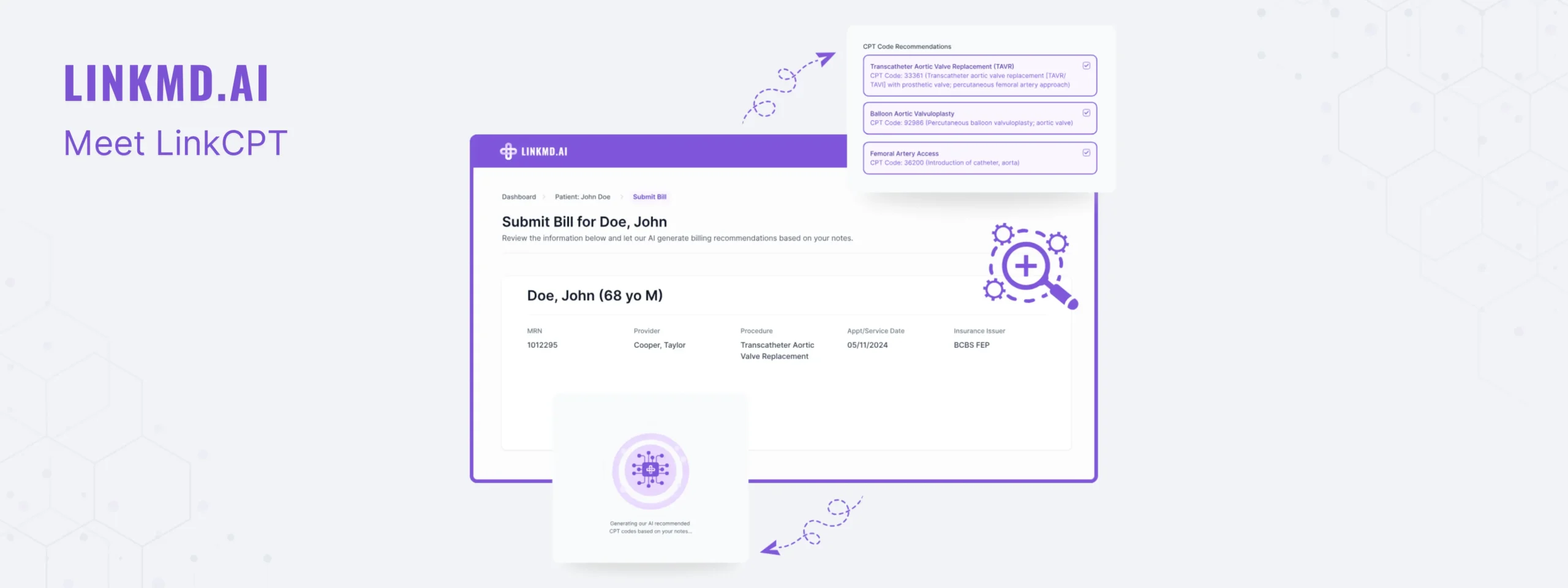
An innovator in the digital health ecosystem, LinkMD is on a mission to redefine how payers, providers, and patients navigate the complexities of prior authorization. By combining smart data exchange and AI-assisted analytics, LinkMD simplifies approvals while preserving the human insights that remain critical in clinical decision-making. Some of the ways LinkMD and similar platforms are driving change include:
- Real-time Collaboration: Giving providers and payers instant visibility into authorization status, required documentation, and next steps.
- Predictive Modeling: Flagging incomplete or error-prone requests before they are submitted, thereby preventing denials down the line.
- Seamless Integration: Meeting providers where they already work by integrating directly with major EHR systems, mitigating the hassle of toggling between multiple dashboards.
Benefits for Providers, Payers, and Patients
When prior authorization is optimized with cutting-edge technology, everyone benefits:
- Providers reduce manual work and burnout, leading to more time with patients.
- Payers see fewer incoming errors and faster turnarounds, increasing overall efficiency.
- Patients experience quicker approvals, less confusion, and uninterrupted access to necessary care.
Looking Ahead: The Future of Prior Authorization
From Reactive to Proactive
Tomorrow’s prior authorization process will go beyond merely streamlining administrative functions; it will proactively shape the clinical journey. Intelligent systems armed with comprehensive patient data can anticipate authorization needs before they arise, providing recommendations in real time to clinicians during the care planning phase.
Continuous Learning and Personalized Care
As AI algorithms learn from each case, they will begin to glean insights that further personalize care and approvals. By identifying patterns in outcomes and payer requirements, technology can suggest the best diagnostic tests, treatment protocols, and authorization approaches for each individual patient. Over time, these machine-driven insights will help close care gaps, reduce errors, and enhance patient outcomes.
Enhanced Transparency and Collaboration
We can also anticipate improved transparency in prior authorization, where patients can track their request status just as easily as they track an online shipment. Providers and payers will continue collaborating more closely, evolving the system into a truly patient-centric model. In this future state, technology empowers faster decisions, fewer denials, and more trust.
Conclusion
The future of prior authorization holds significant promise, fueled by the advancements of automation, AI, and data interoperability. These digital transformations do more than just speed up paperwork; they pave the way for a healthcare system that is more efficient, more transparent, and more attuned to the unique needs of each patient.
By embracing these emerging solutions—including innovations from organizations like LinkMD—providers and payers can finally break free from the outdated, cumbersome processes that have stifled progress for so long. The result? A healthcare experience that is simpler, more intuitive, and ultimately better for all parties involved.
The era of frustrating, time-consuming prior authorization is ending. In its place is a future where technology ensures rapid approvals, minimal administrative strain, and improved patient care—a future that is already within our reach.